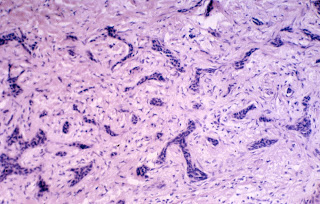
Infiltrative Basal Cell Carcinoma
Think of nodular basal cells as cauliflower. When you thin slice cauliflower, the slice looks like individual balls of material, but in actuality they were attached to the main stalk of the cauliflower. Infiltrative basal cells, on the other hand, extend as worm holes down into the tissue, and the way to think of them in 3-D is as if you were thin slicing a mass of cold spaghetti. if you looked at only the thin slice, it would look almost exactly like this slide: some of the strands would be viewed straight on, others are cut at an angle so as to give the appearance of little spikes and strands of tissue.
Why bother with this? Because once you get the "zen" of this tumor, you will be able to understand how to defeat it. The best way, by far, is by Mohs surgery. We can track down all the individual strands and tentacles that extend form the main body of the tumor, and that will give you the highest cure rate. But, you say, I don't do Mohs! Well, you can either take a wide margin around what you see as the edge of the tumor, or you can use a little trick: Stretch the skin, and look for blanching, Since the tumor is a space-occupying lesion in the dermis, it displaces blood vessels and so when you stretch the skin around the tumor, it blanches out the skin where the tumor is. That is a more accurate way of predicting the margin. Many of you are doing surgeries, and when you are approaching basals and SCCs it is helpful to define the margins as well as you can. Along with stretching the skin, also consider curetting the tissue prior to excision for nodular BCCs and SCCs. It'll cut way down on your positive margin rate. On infiltratives, that won't work because the strands of tumor are too small for the curette to be able to adequately define.
The clinical differential diagnoses for these infiltrative tumors are scars, microcystic adnexal carcinomas, a benign growth known as a desmoplastic trichoepithelioma, and the occasional weird large syringoma. If the infiltrative tumor has increased collagen under the microscope, it is known as "sclerosing", which means "scarring".
Small clinical tumors can be very large:
Infiltrative BCC post-Mohs
One final point: nodular basals can be triggered into becoming infiltrative with external trauma, such as consistent scratching, or from partial treatment, especially by using liquid nitrogen on nodular and superficial BCCs. It is imperative that you biopsy what you don't know, and only freeze those lesions that you KNOW are actinic keratoses.

No comments:
Post a Comment